Dispensing surgical dressings in your office can improve outcomes, patient satisfaction, and can result in tremendous profits. The main surgical dressings that can be dispensed include:
With many options, it can be difficult to select the best option. In last week’s blog, we looked closely at AMERIGEL® Hydrogel Wound Dressing. This week, we are going to investigate AMERX® Hydrocolloid Dressing.
Hydrocolloid Indication
An important tenant of wound care is moisture balance. The goal is always to maintain a moist healing environment without allowing the wound bed to become too moist, or too dry. When a wound has excess moisture, this can be addressed with foam or calcium alginate. However, the opposite situation may exist, where the wound bed is too dry. This can delay healing, increase the risk of complications, and contribute to undesirable scarring. In this situation, hydrocolloids can be used to create a moist wound environment. AMERX Hydrocolloid Dressing is occlusive and water-resistant. In this state, it is also impenetrable to bacteria and supports autolytic debridement. AMERIGEL Hydrogel Wound Dressing introduces moisture without occlusion, whereas AMERX Hydrocolloid Dressing is an option for creating a moist wound environment with occlusion.
Combining with Other Dressings
Hydrocolloid dressings can serve as either a primary dressing or a secondary dressing. When using as a primary dressing, hydrocolloid is applied directly to the wound bed. As a secondary dressing, hydrocolloid can be used to cover and secure a primary dressing in place. For example, collagen powder can be used as the primary dressing and hydrocolloid as the secondary dressing. These items are often dispensed together for wounds with light drainage. The requirement for the wound to have light drainage is common to both collagen and hydrocolloid.
Documentation Requirements
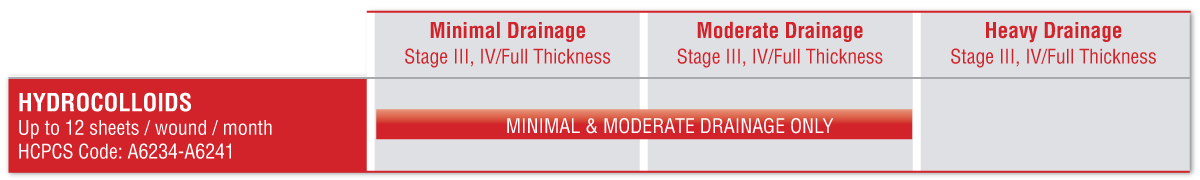
Beyond establishing medical necessity, the documentation must also include that the wound being treated has “light to moderate” exudate for hydrocolloid to be covered by the DMEMACs. Hydrocolloid is not covered if the note does not include the medical necessity of the dressing, or if the documentation indicates heavy exudate is present. Even after payment is made, recoupments can occur if inadequate documentation is discovered later.
Conclusion
Hydrocolloid creates a moist wound environment to wounds with “light to moderate exudate”. DMEMAC coverage allows up to 12 hydrocolloid dressings per month per ulcer when medically necessary. In addition to providing moisture, the occlusion of the hydrocolloid dressing is also impenetrable to bacteria and supports autolytic debridement.
DISCLAIMER: The information provided here is intended to educate health care providers regarding compliance with ICD, CPT, and HCPCS coding. The information provided does not guarantee reimbursement and is accurate to the best of our knowledge at the time of this publication. Coding guidelines can change and we encourage you to stay up to date. The existence of a code does not guarantee payment.

Dr. Jeffrey D. Lehrman, DPM, FASPS, MAPWCA, CPC, CPMA
Dr. Lehrman is a podiatrist practicing in Fort Collins, CO and operates Lehrman Consulting, LLC which provides consultation services regarding coding, compliance and documentation. Dr. Lehrman is a Certified Professional Coder and Certified Professional Medical Auditor. He serves as a staff liaison at the AMA CPT® Editorial Panel meetings where CPT codes are created, edited, and deleted. He is a Diplomate of the American Board of Foot and Ankle Surgery, Fellow of the American Society of Podiatric Surgeons, and is recognized as a “Master” by the American Professional Wound Care Association. Dr Lehrman is a Fellow of the American Academy of Podiatric Practice Management, Past Director of the American Professional Wound Care Association Board of Directors, and is a Past Chairman of the Board of the American Society of Podiatric Surgeons. Dr. Lehrman is also on the editorial advisory board of the journal WOUNDS.