Lymphedema can be a crippling and painful disease if not appropriately treated. Now, there is a treatment option that works, is comfortable, and is tolerated well by patients, the EXTREMIT-EASE from AmerX. More good news: Medicare coverage for this treatment expanded significantly starting January 1, 2024.
Lymphedema
Lymphedema is the result of an abnormal accumulation of lymph fluid. Lymph fluid carries cells that help to prevent and fight infection. Cells that help to prevent and fight infection are typically beneficial. However, too much lymph fluid can cause problems. An excess of lymph fluid can develop when lymph vessels are damaged and / or when lymph nodes are not functioning properly. Lymph vessels are supposed to transport lymph fluid to where it is intended to be, but if these lymph vessels are not functioning properly, the lymph fluid can end up where it does not belong. Lymph nodes are supposed to help regulate the amount of lymph fluid in the body and if they are not functioning properly, too much lymph fluid can accumulate.
There are two main types of lymphedema:
Primary Lymphedema – Congenital, meaning it was present at birth or develops later in life without any known cause or inciting incident
Secondary Lymphedema – Develops as a result of an insult to lymph nodes and / or lymph vessels. A common cause of secondary lymphedema is cancer surgery that results in the damage of or removal of lymph nodes and / or lymph vessels. Radiation treatment can also negatively affect the function of lymph nodes and / or lymph vessels leading to secondary lymphedema.
In other instances, it is possible for a cancerous tumor to get so large that it causes an obstruction (blockage) in the lymphatic system.
Most providers consider there to be four stages of lymphedema:
Stage One – Abnormal function of the lymphatic system that may have no outward signs or symptoms
Stage Two – Minimal swelling that may be alleviated by elevation or compression
Stage Three – Swelling of an area that does not resolve with elevation. There may be skin thickening and scarring.
Stage Four – Severe swelling and skin abnormalities
Complications of Lymphedema
Complications of lymphedema also include: |
|||
|
|
||
|
|
||
|
|
||
|
|
||
|
|
||
Lymphedema Versus Chronic Venous Insufficiency
While lymphedema is an abnormal accumulation of lymph fluid, chronic venous insufficiency is an abnormal accumulation of blood. Veins are responsible for returning blood back to the heart. In chronic venous insufficiency, the veins of the legs do not function properly and blood is not returned to the heart the way it should be. When this happens, blood can stay in the legs instead of being returned to the heart. Sometimes the blood even flows backwards and ends up collecting in the legs. When blood is not returned from the legs, and instead stays in the legs, it is called venous stasis. When evaluating swelling of the legs it is important to differentiate between lymphedema and chronic venous insufficiency.
|
“ |
While lymphedema is an abnormal accumulation of lymph fluid, chronic venous insufficiency is an abnormal accumulation of blood. |
Lymphedema Treatment
There is no cure for lymphedema. However, it can be managed when the appropriate tools are employed. When lymphedema is appropriately managed, the risks of the complications listed above occurring are significantly decreased.
Extermit-EASE changes all of that with a revolutionary design that makes it much easier for patients to apply, remove, and tolerate. Extremit-EASE combines a zipper and bungees with large tabs to make independent application and adjustment easy for patients to achieve—even if they suffer from dexterity issues. Patients appreciate the lightweight, air permeable fabric allowing for hours of comfortable wear with less sweat, fewer hot spots, and less pistoning.

An air permeability study demonstrated that Extremit-EASE provides between 3 and 11 times the amount of air permeability than more traditional options. This supports the fact that the lightweight, air permeable fabric of Extremit-EASE contributes to fewer problems with experiencing heat and other discomfort when using Extremit-EASE.
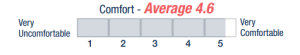
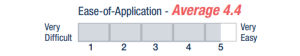
Another study[1] demonstrated the marked difference in compliance with compression when the Extermit-EASE is used. This study truly tested the improvement when Extremit-EASE is selected over other options by only including patients with venous insufficiency or lymphedema who had failed treatment with standard compression because they could not tolerate it. On a scale of 1-5, with 1 being “very difficult” and 5 being “very easy,” patients in the study ranked “ease of application” with the more traditional compression garment as 1.74 versus 4 with Extremit-EASE. On a scale of 1-5, with 1 being “very uncomfortable” and 5 being “very comfortable,” patients in the study ranked “comfort” with the more traditional compression garment as 1.91 versus 4.17 with Extremit-EASE. The patients in this study were able to wear the Extremit-EASE almost twice as many hours per day as they did the more traditional option. Better compliance by patients with the treatment they need results in better results for them and better outcomes for medical practices[2].
[1] “Does the Use of Velcro-Bungee Compression Garment Improved Patient Experience and Compliance with Compression Therapy?” C. Jake Lambert, Jr MD, CWSP; Jason M McLeod, CWCA; Christopher L Rodriguez, PA-C; Wendy L Smiley, CSFA; Cameron Lambert, BS
[2] Compression for preventing recurrence of venous ulcers. Nelson EA, Bell-Syer SE, Cullum NA Cochrane Database Syst Rev. 2000; (4):CD002303.
Lymphedema Coverage
In order to make this change, a new benefit category was added to the Social Security Act. In making this change, the Centers for Medicare and Medicaid Services (CMS) acknowledged that “gradient compression garments are effective in reducing and/or preventing progression of lymphedema in the arm and leg” and that gradient compression garments are “effective in maintaining limb circumference.” This new coverage includes both standard fit garments, such as the EXTERMIT-EASE, and custom-fit garments. Standard fit compression garments may be referred to as “ready-made” or “ready-to-wear,” are available off-the-shelf, and are typically available in a range of sizes.
According to CMS-1780-F, this new Medicare coverage includes compression garments that are:
- Furnished on or after January 1, 2024, to an individual with a diagnosis of lymphedema for the treatment of such condition;
- Primarily and customarily used to serve a medical purpose and for the treatment of lymphedema, as determined by the Secretary;
- Prescribed by a physician (or a physician assistant, nurse practitioner, or a clinical nurse specialist (as these terms are defined in section 1861(aa)(5)) to the extent authorized under State law).
Medicare coverage for EXTERMIT-EASE compression garments when treating lymphedema now includes up to three medically necessary daytime garments for each affected limb or area of the body every 6 months. The reason three garments are allowed for each affected limb or area of the body is to allow patients to wear one, wash one, and dry one at any given time. The importance of hygiene is stressed in the CMS-1780-F guidance that created this coverage. Furthermore, Medicare coverage of EXTREMIT-EASE when treating lymphedema includes both Phase 1 and Phase 2 treatments.
Phase 1 of lymphedema treatment is often referred to as acute or decongestive therapy. It may also be referred to as the intensive phase of treatment. Phase 1 may include wraps with long-stretch and / or short-stretch bandaging.
Phase 2 is often referred to as the “maintenance phase.” The goal during Phase 2 of treatment is to maintain the progress made during Phase 1 and prevent recurrence. Lymphedema is typically a lifelong issue and patients who are in Phase 2 of treatment normally strive to remain in Phase 2 for the rest of their lives without reverting to the need for Phase 1 treatment. These patients typically have to wear gradient compression garments all day long forever to prevent worsening.
Lymphedema Coverage Versus Chronic Venous Insufficiency Coverage
While Medicare coverage of EXTREMIT-EASE for lymphedema is outlined in CMS-1780-F, Medicare coverage of EXTREMIT-EASE for chronic venous insufficiency is different and outlined in the Durable Medical Equipment Medicare Administrative Contractor (DMEMAC) Local Coverage Determination “Surgical Dressings” (L33831) and the DMEMAC Policy Article “Surgical Dressings” (A54563). In these policies, when EXTREMIT-EASE is used for chronic venous insufficiency, Medicare only allows coverage when it is used in the treatment of an “open venous stasis ulcer” that meets the qualifying wound requirements of the Surgical Dressing policies. Thus, the coverage for EXTREMIT-EASE is very different depending on whether it is being used for lymphedema or it is being used for chronic venous insufficiency.
Coding
With this Medicare coverage change, there are now two different codes for the same EXTREMIT-EASE garment, with selection based on whether it is being used to address lymphedema or if it is being used to address chronic venous insufficiency with an open venous stasis ulcer. When used to address lymphedema, the EXTREMIT-EASE HCPCS code is A6583 (Gradient compression wrap with adjustable straps, below knee, 30-50 mmhg, each). When used to treat chronic venous insufficiency with an open venous stasis ulcer, the EXTREMIT-EASE HCPCS code is A6545 (Gradient compression wrap, non-elastic, below knee, 30-50 mmhg, used as a surgical dressing).
|
“ |
When used to address lymphedema, the EXTREMIT-EASE HCPCS code is A6583 |
|
“ |
When used to treat chronic venous insufficiency with an open venous stasis ulcer, the EXTREMIT-EASE HCPCS code is A6545 |
Lymphedema Diagnosis Codes
Common ICD-10-CM codes that represent lymphedema include:
- Lymphedema, not elsewhere classified (I89.0)
- Hereditary Lymphedema (Q82.0)
- Postmastectomy Lymphedema Syndrome (I97.2)
- Other postprocedural complications and disorders of the circulatory system, not elsewhere classified (I97.89)
I97.89 should only be selected if the patient is experiencing postprocedural complications and / or disorders of the circulatory system that do not have their own, more specific, ICD-10-CM code.
Documentation
As is the case with any service or product, when EXTREMIT-EASE is dispensed to treat lymphedema, the medical necessity of the item must be documented This includes documenting the pathology being addressed and why the EXTREMIT-EASE compression garment is medically necessary. An example of this documentation of medical necessity is:
|
“ |
As a result this lymphedema, this patient has an abnormal accumulation of lymphatic fluid in their ___ leg. This creates risk for infection, ulceration, and other skin issues. This can also lead to pain and potentially impact ambulation. It can even lead to lymphangiosarcoma. I explained to the patient that there is no cure for lymphedema and also explained the need for treatment. Treatment in the form of compression is medically necessary to reduce swelling here and to help reduce the risk of potential lymphedema complications. This lymphedema requires compression. This compression is best achieved with a daytime gradient compression garment that offers graduated, consistent compression. To optimize outcomes and best prevent complications, this patient should be generally wearing this garment all day every day. Therefore, it was medically necessary to dispense three garments per affected leg so the patient has one to wear, wash, and dry each day. |
This is only an example of documentation. Of course, medical record documentation should be specific to the patient treated during the encounter and should describe the pathology encountered that day. In addition to this statement of medical necessity, the medical record should also contain a detailed history and physical exam that supports the diagnosis of lymphedema when it is present.
Other Documentation
As EXTREMIT-EASE is still durable medical equipment when dispensed for lymphedema, there are other documentation requirements that must be met. Providers should document the number of items dispensed, which body part it will be used on including laterality, and the size of the items dispensed. Instructions for use should also be documented, including how the patient was told to use the item and the frequency with which it will be used. Supplier standards and warranty information should be provided to the patient and the fact that these were provided should be documented. The Proof of Delivery must be complete and in the medical record.
|
“ |
In the case that the provider is both the prescriber and the supplier, a separate Standard Written Order is not required if all of its required elements exist within this progress note. |
The Proof of Delivery must include the patient’s name, address where item was delivered, description of the item, quantity delivered, patient or designee signature, and date delivered. A Standard Written Order should also be complete and in the medical record. In the case that the provider is both the prescriber and the supplier, a separate Standard Written Order is not required if all of its required elements exist within this progress note. These required elements of the Standard Written Order include the beneficiary’s name or Medicare beneficiary identifier number, order date, description of the item (can be general description, a HCPCS code, a HCPCS code narrative, or a brand name/model number), quantity to be dispensed, treating practitioner’s name or NPI, and the treating practitioner’s signature. Even though there is overlap in the required elements of the Proof of Delivery and Standard Written Order, both must be separately completed.
Conclusion
Lymphedema is a relatively common condition that is typically treatable with the convenient and comfortable EXTREMIT-EASE compression garment. Medicare coverage for gradient compression garments used for lymphedema expanded in 2024 and now includes treatment in the absence of an open ulcer.

Dr. Jeffrey D. Lehrman, DPM, FASPS, MAPWCA, CPC, CPMA
Dr. Lehrman is a podiatrist practicing in Fort Collins, CO and operates Lehrman Consulting, LLC which provides consultation services regarding coding, compliance and documentation. Dr. Lehrman is a Certified Professional Coder and Certified Professional Medical Auditor. He serves as a staff liaison at the AMA CPT® Editorial Panel meetings where CPT codes are created, edited, and deleted. He is a Diplomate of the American Board of Foot and Ankle Surgery, Fellow of the American Society of Podiatric Surgeons, and is recognized as a “Master” by the American Professional Wound Care Association. Dr Lehrman is a Fellow of the American Academy of Podiatric Practice Management, Past Director of the American Professional Wound Care Association Board of Directors, and is a Past Chairman of the Board of the American Society of Podiatric Surgeons. Dr. Lehrman is also on the editorial advisory board of the journal WOUNDS.





